Published by CanvasRebel
We were lucky to catch up with Dr. Buffy Lloyd-Krejci recently and have shared our conversation below.
Alright, Dr. Buffy thanks for taking the time to share your stories and insights with us today. Have you ever experienced a time when your entire field felt like it was taking a U-Turn?
There is no question the nursing home industry is facing a “U-Turn” moment right now! In the midst of the COVID pandemic and studying the spread of infectious diseases in nursing homes in the United States, I discovered extreme disparities. Even before the pandemic, between one and three million infections resulted in 380,000 deaths among nursing home residents each year. There was little to no resources for infection prevention and control practices, leaving these institutions in a vulnerable position when the pandemic hit. People often have the wrong idea about nursing homes. This is no surprise as they are often vilified and blamed instead of supported. In February, President Biden called on Congress to provide $500 million to fund the Centers for Medicare and Medicaid Services health and safety inspection in nursing homes. In my book, Broken, I describe the underlying issues, but offer a better way than just throwing money at the ineffective regulatory system.
Dr. Buffy, love having you share your insights with us. Before we ask you more questions, maybe you can take a moment to introduce yourself to our readers who might have missed our earlier conversations?
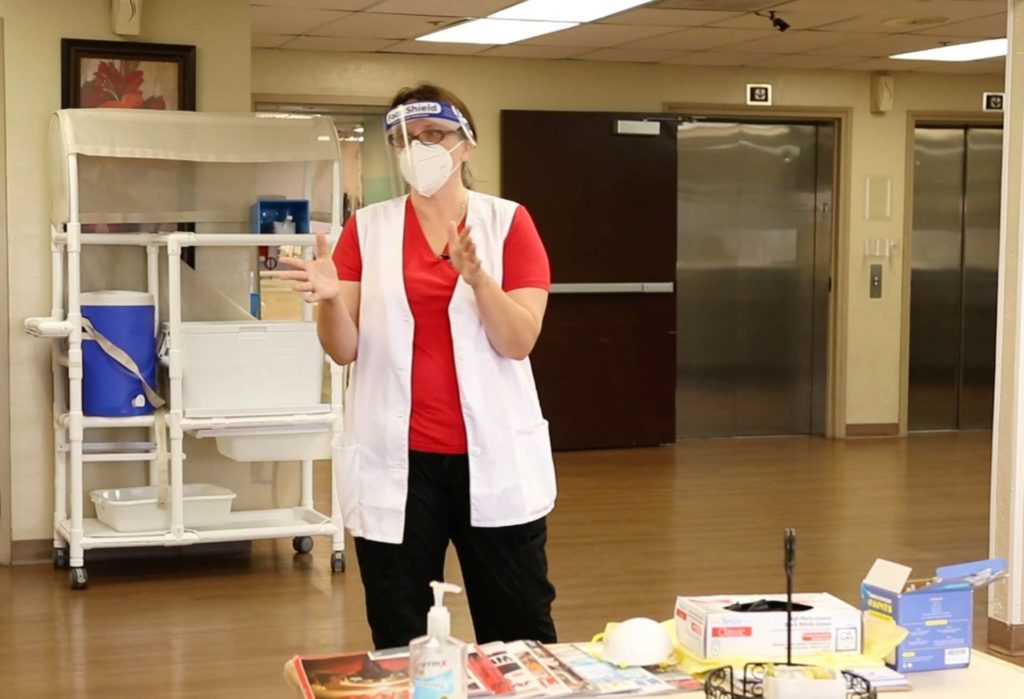
I’m one of the foremost authorities on infection prevention and control in nursing homes and long-term care facilities. I have been a frequent contributor and interview source for the national and trade press concerning infection prevention and control and mitigation. Recently, I decided to write the book “Broken: How the Global Pandemic uncovered a nursing home industry in need of repair and heroic staff fighting for change,” and it was published on April 12, 2022. My practice, IPCWell is headquartered in the Phoenix metropolitan area and is devoted to mitigating infectious diseases and inappropriate antibiotic prescribing in all healthcare settings to reduce adverse events, infections, antibiotic resistance, re-admissions, and death. I have consulted with health care facilities across the United States and with international humanitarian groups (Doctors Without Borders).
With more than 20 years of healthcare & public health experience, I pride myself on the fact that my data-driven approach is hands-on and collaborative. Using my experience with more than 200 nursing homes across the United States, I work tirelessly to combat the estimated one to three million infections leading to more than 380,000 deaths every year in the nursing home industry. Having worked with the CDC and other organizations on infection control studies and research such as the Arizona emergency Preparedness Infection Control (EPIC) grant, the Institute of Health Project ECHO, a hub-and-spoke knowledge-sharing network to support NH leadership during COVID-19, and the first ever US based mission with Doctors Without Borders in Detroit, Michigan and Houston, Texas. Previously, I worked as a Quality Improvement Advisor on Healthcare Acquired Infections with Health Services Advisory Group, conducted research as a Research Assistant with the Mayo Clinic in Arizona, and have served as Hospital Unit Coordinator for Arrowhead Hospital, Straub Clinic & Hospital, and Banner Good Samaritan Hospital.
Any advice for growing your clientele? What’s been most effective for you?
The most effective strategy for growing my clientele has been a mixture of building good relationships and word-of-mouth. I worked with hundreds of healthcare facilities during my time working for the Quality Improvement Network-Quality Improvement Organization, back in 2015, and that was my foundation. Once I formed relationships with healthcare providers, I started to hear from other administrators, DONs, and infection preventionist at facilities that I hadn’t even gone to, but they’d heard what I had been doing to support other facilities. They knew that we were doing good work and they wanted me to come and help them implement evidence-based infection prevention and control practices within their facility. I know these methods are old-fashioned, but it really does work to just build a good relationship and reputation with clients and let that reputation speak for itself.
Training and knowledge matter of course, but beyond that what do you think matters most in terms of succeeding in your field?
As with any field, human relationship is key to success in my work with healthcare facilities, both for training and for the ultimate reform that is needed. The many years of training and education that I went through gave me a solid foundation to build my career, but the thing that allows me to have a real impact is connecting with the people I get to work with. Healthcare workers are passionate, caring people that too often lack the resources they need to really serve their patients. By creating deep relationships with them, I get to hear their struggles, provide support, and go out into the world to fight for real change.