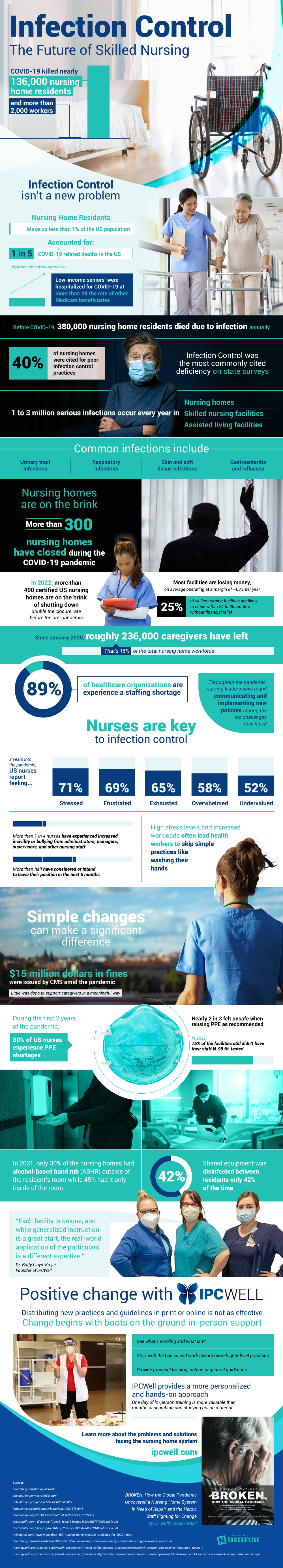
It’s no secret that nursing homes shouldered the brunt of the damage during the pandemic. Residents, and even staff, had a hugely disproportionate number of COVID deaths compared to the rest of the U.S. populace. But what you may not have known is that during their struggle to keep residents safe, during a literal fight for their lives, ever-changing regulations and punitive measures were mounted against them rather than support and relief. Infection prevention and control is an aspect of this industry that will save countless lives when ingrained into the fundamentals of care. Learn more about how we must implement these protocols and offer whatever support we can to get them into place to ensure a safe and healthy future for an industry that we may not be near today, but will touch all of our lives eventually.
The Future Of Skilled Nursing
COVID-19 killed nearly 136 000 nursing home residents and more than 2000 workers Infection Control Isn’t A New Problem- 1 in 5 COVID-19 related deaths in the US
- Nursing home residents make up less than 1% of the US population
- Low-income seniors (eligible for both medicare and medicaid) were hospitalized for COVID-19 at more than 4X the rate of other Medicare beneficiaries
- Before COVID-19, 380,000 nursing home residents died due to infection each year
- 40% of nursing homes were cited for poor infection control practices
- Infection control was the most commonly cited deficiency on state surveys
- 1 to 3 million serious infections occur every year in
- Nursing homes
- Skilled nursing facilities
- Assisted living facilities
- Common infections include
- Urinary tract infections
- Respiratory infections
- Skin and soft tissue infections
- Gastroenteritis and influenza
- Nursing Homes Are On The Brink
- More than 300 nursing homes have closed during the COVID-19 pandemic
- In 2022, more than 400 certified US nursing homes are on the brink of shutting down – double the closure rate before the pandemic
- Most facilities are losing money, on average operating at a margin of -4.8% per year
- 25% of skilled nursing facility are likely to close within 24 to 36 months without financial relief
- Roughly 236,000 caregivers have left since January 2020
- That’s 15% of the total nursing home workforce
- 89% of healthcare organizations are experience a staffing shortage – 54% say it’s a serious problem
- More than 300 nursing homes have closed during the COVID-19 pandemic
- 2 years into the pandemic, US nurses report feeling
- Stressed: 71%
- Frustrated: 69%
- Exhausted: 65%
- Overwhelmed: 58%
- Undervalued: 52%
- 1 in 4 facilities reported shortages in nursing staff
- More than 1 in 4 nurses have experienced increased incivility or bullying from administrators, managers, supervisors, and other nursing staff
- More than half of have considered or intend to leave their position in the next 6 months
- Simple Changes Can Make A Significant Difference
-
-
- $15 million dollars in fines were issued by CMS amid the pandemic
- Little was done to support caregivers in a meaningful way
- During the first 2 years of the pandemic, 80% of US nurses experience PPE shortages
- Nearly 2 in 3 felt unsafe when reusing PPE as recommended
- $15 million dollars in fines were issued by CMS amid the pandemic
-
- In 2021, 75% of the facilities still do not have their staff N-95 fit-tested
- In 2021, only 30% of the nursing homes had alcohol-based hand rub (ABHR) outside of the resident’s room while 45% had it only inside of the room
- Shared equipment was disinfected between residents only 42% of the time
- Distributing new practices and guidelines in print or online doesn’t work – Change begins with in-person support
- See what’s working and what isn’t
- Start with the basics and work toward more higher level practices
- Provide practical training instead of general guidelines
- IPCWell provides a more personalized and hands-on approach
- One day of in-person training is more valuable than months of searching and studying online material
